As the autumn season sets in and the crisp air has many people heading to their local cider mills and farmers’ markets, officials with the FDA are reminding consumers about the potential problems that have been associated with drinking juice and cider that have not been pasteurized.
As the autumn season sets in and the crisp air has many people heading to their local cider mills and farmers’ markets, officials with the FDA are reminding consumers about the potential problems that have been associated with drinking juice and cider that have not been pasteurized.
Many local markets will sell packaged juice that was made on site and has not been pasteurized or otherwise processed to ensure its safety. Serious outbreaks of foodborne illness have been linked to these beverages, according to agency officials.
If a product has been untreated, it should be kept refrigerated and carry the following warning label:
“WARNING: This product has not been pasteurized and therefore may contain harmful bacteria that can cause serious illness in children, the elderly, and persons with weakened 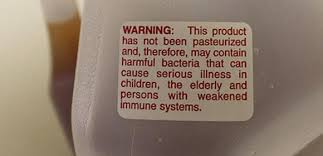 immune systems.”
immune systems.”
However, the FDA does not require warning labels on juice or cider that is fresh-squeezed and sold by the glass such as at apple orchards and roadside stands.
Consumers should follow these steps to help prevent illness associated with untreated juice and cider:
- Look for the warning label to avoid the purchase of untreated juices. Untreated juice is most likely to be sold in the refrigerated section of a grocery store.
- Don’t hesitate to ask if unsure if a juice product is treated, if the labeling is unclear, or if the juice or cider is sold by the glass.
Consuming dangerous foodborne bacteria will usually cause illness within 1 to 3 days of  eating the contaminated food. However, sickness can also occur within 20 minutes or up to 6 weeks later. Symptoms of foodborne illness include: vomiting, diarrhea, abdominal pain, and flu-like symptoms
eating the contaminated food. However, sickness can also occur within 20 minutes or up to 6 weeks later. Symptoms of foodborne illness include: vomiting, diarrhea, abdominal pain, and flu-like symptoms
Source: FDA