The Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) of the US Food and Drug Administration (FDA) gave the thumbs-up today to recommending, for the first time, approval for a new class of medications: proprotein convertase subtilisin kexin 9 (PCSK9) inhibitors.
The Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) of the US Food and Drug Administration (FDA) gave the thumbs-up today to recommending, for the first time, approval for a new class of medications: proprotein convertase subtilisin kexin 9 (PCSK9) inhibitors.
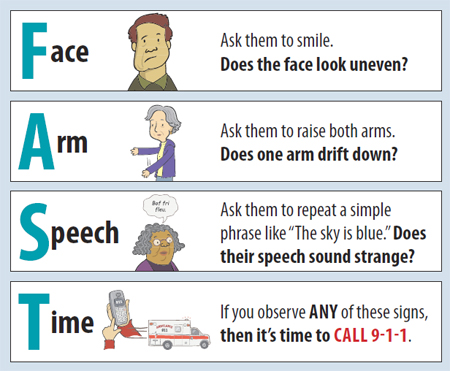
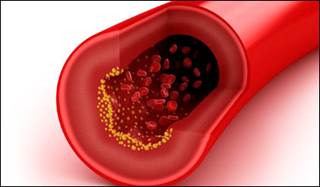
They voted 13 to 3 in favor of alirocumab (Praluent,  Sanofi/Regeneron) for lowering LDL cholesterol in patients with hypercholesterolemia, citing likely benefit especially for patients with heterozygous familial hypercholesterolemia (HeFH). Other groups predicted to get special benefit to include those at high CV risk or who don’t tolerate statins. Although there was a lot of debate without consensus about these latter groups, the vote just focused on whether the drug’s benefits exceeded its risks to support approval “in one or more patient populations.”
Sanofi/Regeneron) for lowering LDL cholesterol in patients with hypercholesterolemia, citing likely benefit especially for patients with heterozygous familial hypercholesterolemia (HeFH). Other groups predicted to get special benefit to include those at high CV risk or who don’t tolerate statins. Although there was a lot of debate without consensus about these latter groups, the vote just focused on whether the drug’s benefits exceeded its risks to support approval “in one or more patient populations.”
The biggest discussion of the day was whether the drug should be approved based only on its effect on LDL-C—even before its CV-outcomes trial has been completed. Many panel members, including chair Dr Robert J Smith (Alpert Medical School of Brown University, Providence, RI), did not agree that LDL-C lowering is 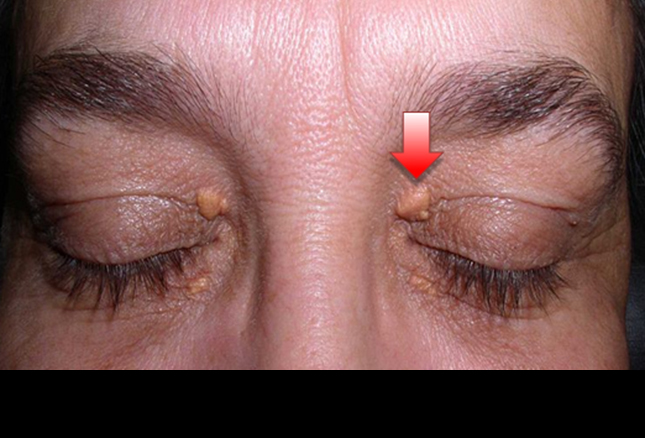 sufficient for establishing effectiveness for reducing CV risk. “I just don’t think it predicts clinical outcomes. I would need to see the clinical outcomes,” he said.
sufficient for establishing effectiveness for reducing CV risk. “I just don’t think it predicts clinical outcomes. I would need to see the clinical outcomes,” he said.
However, Smith was among the “yes” votes today, noting that patients with HeFH really need this drug—a point that came out throughout all discussions. During the public-hearing session, 14 of 16 speakers gave strong approval for the medication, with most sharing stories of how they and/or family members have struggled with this disorder.
Source: Medscape