 The US Food and Drug Administration (FDA) is warning consumers that fraudulent treatments for Ebola virus disease are being marketed online.
The US Food and Drug Administration (FDA) is warning consumers that fraudulent treatments for Ebola virus disease are being marketed online.
Although some experimental therapies and vaccines are in early phases of development, no products for treating Ebola infection have been approved by the FDA. So far, only limited data are available about the safety and effectiveness of the products being tested, and only small supplies are available, according to the agency. Experimental therapies were used to treat 2 US health care workers who were moved to Atlanta after they became infected by Ebola virus while caring for patients in West Africa, where there is an ongoing outbreak.
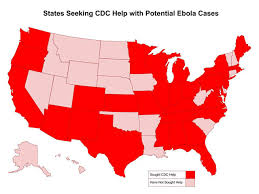
The US Center for Disease Control and Prevention says there is little threat of Ebola spreading in the United States. But some online marketers have seized on global concern about the illness to sell fraudulent products, according to the FDA. It is illegal for companies to market unapproved products claiming to cure or prevent disease. The FDA is asking the public to report suspect claims about Ebola-related products (https://1.usa.gov/1mS3T3P).
marketers have seized on global concern about the illness to sell fraudulent products, according to the FDA. It is illegal for companies to market unapproved products claiming to cure or prevent disease. The FDA is asking the public to report suspect claims about Ebola-related products (https://1.usa.gov/1mS3T3P).
(JAMA)
Read more here.
The Presidential Healthcare Center’s preventative programs include emergency preparedness advice to keep you safe and healthy no matter where you travel.