People with moderate-to-severe vitamin D deficiencies are significantly more likely to develop Alzheimer’s disease or other forms of dementia than those who have an adequate supply of the vitamin in their body, a new study has found.
Researchers, led by David J. Llewellyn at the University of Exeter Medical School, found that adults who suffered from a moderate deficiency of vitamin D had a 53 percent higher risk of some form of dementia, while the risk increased 125 percent in those with severe deficiencies. People moderately deficient in vitamin D were 69 percent more likely to develop Alzheimer’s-caused dementia, while those severely deficient raised the risk to 122 percent.
The team discovered what appear to be clear threshold levels for brain health using standard medical measurements of concentration in the blood. The risk of dementia appears to rise for people with vitamin D blood levels below 25 nanomoles per liter, while vitamin D levels above 50 nanomoles appear to be good levels for brain health.
Llewellyn said that although the international team of researchers expected to find a link between vitamin D deficiency and dementia, the strong correlation between the two was surprising. He said further study was necessary to determine whether consuming oily fish or vitamin D supplements might prevent Alzheimer’s disease.
Alzheimer’s disease is the leading form of dementia, affecting more than 5 million people in the United States. That number is expected to reach 16 million by 2050 as the population ages.
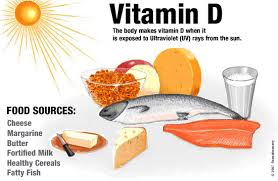
Vitamin D, which helps the body use calcium, is created when skin is exposed to sunshine. Milk is often fortified with the vitamin, and it is also found in fatty fish and other foods.
Researchers in the Exeter study noted that laboratory experiments have shown that vitamin D may play a role in ridding cells of beta-amyloid plaques, an abnormality that distinguishes Alzheimer’s.
“It seems to be that vitamin D was actually helping to break down and take away those protein abnormalities,” Llewellyn said Wednesday in an interview.
The study, funded in part by the Alzheimer’s Association, appeared Wednesday in Neurology, the medical journal of the American Academy of Neurology.
Source: Washington Post