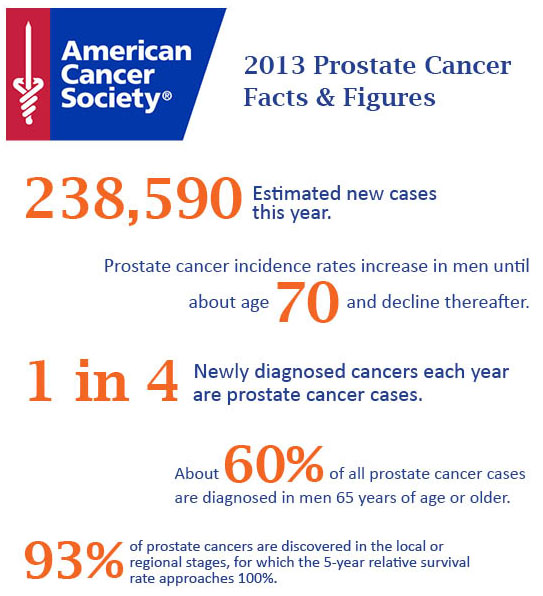
For the first time, updated results from the European Randomized Study of Screening for Prostate Cancer (ERSPC), the largest randomized prostate cancer screening trial in the world, show a significant survival advantage with prostate-specific antigen (PSA) screening for men from 50 to 74 years of age.
The new data come from a follow-up of 13 years, and were presented during a late-breaking abstract session here at the European Association of Urology 29th Annual Congress. An initial analysis of the ERSPC results, reported in 2009, provided the first proof that PSA screening saves lives from prostate cancer.
This update “offers the most robust data yet in support of the effectiveness of PSA-based early detection efforts to reduce prostate cancer metastases and mortality,” said Matthew Cooperberg, MD, MPH, associate professor of urology, epidemiology, and biostatistics at the University of California, San Francisco, who was asked by Medscape Medical News for comment.
According to Dr. Cooperberg, who was not involved in the research, the ERSPC, together with the Göteborg trial “provides the only contemporary insights on the question of benefits of early detection.”
He said that the screening study conducted in the United States — the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial — “is now broadly acknowledged only to address the question of annual vs opportunistic screening, given a screening rate of more than 75% in the usual care arm.”
The updated ERSPC results were presented by Jonas Hugosson, MD, professor of urology at the Sahlgrenska Academy, University of Gothenburg, in Sweden. He cautioned that screening with the PSA test “should not start too late,” emphasizing that the weight of screening benefits fall to men whose screening begins before the age of 60.
“In our data from the Göteborg Trial, the Swedish arm of ERSPC, we found a prostate cancer mortality reduction of 20% in men who started PSA screening after age 60, while men who started to screen before age 60 had a reduction of 50%,” Dr. Hugosson told Medscape Medical News.
The ERSPC, which began 20 years ago, was a randomized study of more than 180,000 men, only half of whom underwent regular PSA testing. Results from the 11-year follow-up of the ERSPC were published in 2012.
The gap between screened and unscreened groups is decreasing; the relative risk for prostate cancer between the screening and control groups at 9-year follow-up was 1.91, at 11-year follow-up was 1.66, and at a median of 13 years of follow-up was 1.57, Dr. Hugosson reported.
However, he noted, “we still have a 57% increased incidence of prostate cancer in the screening group, compared with the control group.”
This is one of the downsides of PSA screening — the risk for overdiagnosis of prostate cancer that might not affect the individual’s health in the time he has left to live. However, once it is detected, it might be treated, or at least followed with further screening.
The most recent update from the trial shows that the absolute difference in prostate cancer mortality per 1000 patient-years has increased from 9 years (0.31 vs 0.37) to 11 years (0.35 vs 0.46) to 13 years (0.43 vs 0.54). However, the difference in the relative risk for mortality has stabilized in favor of screening; it was 0.85 at 9 years, 0.78 at 11 years, and 0.79 at 13 years.
The number of men needed to invite for screening to prevent 1 prostate cancer death has decreased from 979 at 9 years and is 781 at 13 years. The number needed to diagnose to prevent 1 death has decreased from 35 at 9 years to 27 at 13 years.
As previously reported by this group, large differences between centers in prostate cancer mortality persist.
“For example, in Finland, our largest center has a 9% mortality reduction, whereas Sweden, our neighbor with the same kind of healthcare system, has more than a 4-fold better mortality reduction (38%),” he said. “The largest mortality reduction was seen in Spain (46%), but an increase in mortality was seen in Switzerland (–14%).
An initial analysis suggested that these differences in outcomes between centers stem from differences in screening protocols, such as rate of biopsy, median PSA per invited man, and duration of screening, which ranged from 4 to 10 years.
“It seems like the intensity of screening is very closely related to the effect of prostate cancer mortality reduction,” he said.
Dr. Cooperberg predicts that the benefits from PSA screening will increase with longer follow-up, and he noted that “for a man in his 50s, the relevant time horizon is 30 years or more, not 13 years.”
“The risk of overdiagnosis with screening is still, of course, very salient,” he explained. “The solution is to focus early detection efforts on the detection of high-risk prostate cancer, with broad implementation of active surveillance as the default strategy for low-risk disease.”
Dr. Cooperberg said he disagrees with efforts to stop or reduce PSA screening in healthy men. “A policy of discouraging all early detection efforts runs counter to the growing body of high-quality evidence, and puts thousands of men at risk of avoidable suffering and early mortality,” he said.
Referring to the 2012 recommendation from the US Preventive Services Task Force (USPSTF) against PSA screening for prostate cancer,he noted that “the USPSTF will update its evidence review in the near future to reflect the increasingly incontrovertible message of the ERSPC: that PSA-based early detection saves lives, period.”
Source: Medscape