Osteoporosis, a loss of bone strength that raises the risk of fractures, is one of the most common and crippling ailments associated with aging in women. Increasingly, it is striking younger patients who have a host of other medical problems.
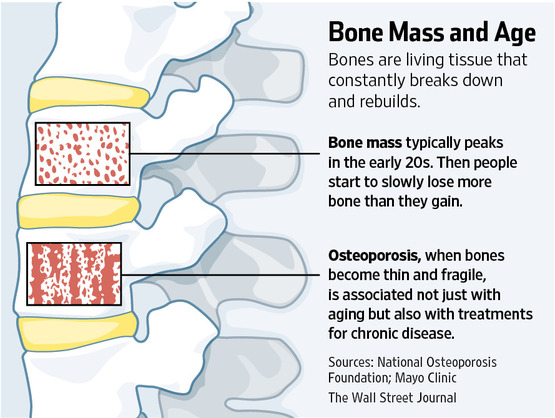
Researchers call it secondary osteoporosis. They are identifying a growing list of factors that contribute to bone deterioration, including chronic diseases and some of the powerful drugs used to treat them. Alone or in combination, disease and medication can interfere with the way the body naturally breaks down and rebuilds bone tissue, and how well it absorbs bone-building nutrients like calcium and Vitamin D.
Because there often are no symptoms as bone weakens, osteoporosis often hasn’t been diagnosed until a patient suffers a fractured bone.
Now, bone health experts are calling for greater efforts to identify patients earlier who are at risk for secondary osteoporosis, before their bones become more fragile and further raise their risk of injury and disability.
Recommended measures include bone mineral density scans for patients who wouldn’t ordinarily get routine screening, treatment of underlying diseases that contribute to bone loss, lifestyle changes and calcium and vitamin D supplements. Doctors also are prescribing osteoporosis medicines shown to slow bone loss or build new bone.
Secondary osteoporosis is increasingly being diagnosed in younger patients with cancer, celiac disease, rheumatoid arthritis and inflammatory bowel disease, as well as in people taking reflux medications, blood thinners and some depression drugs, researchers say. Patients are at risk of secondary osteoporosis after bariatric surgery for weight loss, as are those receiving hormonal treatments to prevent the recurrence of breast or prostate cancer.
Adverse effects of diabetes on bone health are starting to be recognized. Smoking, excessive alcohol use, eating disorders like anorexia nervosa and inactivity are also linked to declining bone mass.
Anyone taking corticosteroids, such as prednisone, is at risk, according to the American College of Rheumatology. The drugs, prescribed to suppress inflammation in a wide range of illnesses and to prevent organ rejection after transplants, have a direct negative effect on bone cells and can interfere with the body’s handling of calcium.
According to the National Osteoporosis Foundation, nine million adults in the U.S. have osteoporosis and an additional 43 million have low bone mass, or osteopenia, which increases their risk of osteoporosis and broken bones. The foundation projects that by 2030, the number of adults over age 50 with osteoporosis and low bone mass will grow by more than 30% to 68 million.
Primary osteoporosis is most commonly caused by women’s loss of estrogen after menopause. Age-related bone loss affects men starting in their 70s.
Last year, a review by researchers at Loyola University Medical Center in Maywood, Ill., found secondary causes of bone loss are reported in up to 60% of men, more than 50% of premenopausal women and some 30% of postmenopausal women who are diagnosed with osteoporosis.
“When I find a younger patient with osteoporosis, there is likely to be a secondary cause, and if that cause isn’t treated, they will continue to lose bone even if they are on osteoporosis medications,” says Pauline M. Camacho, an endocrinologist at Loyola and co-author of the study.
Source: Wall Street Journal